Calcium Metabolism
Introduction :-
Calcium Metabolism- The calcium concentration in the extracellular fluid is normally tightly controlled; it rarely increases or decreases by more than a few percent from the normal value of about 9.4 mg/dl (corresponding to 2.4 millimoles of calcium per liter). This precise control is important because calcium plays a vital role in many physiological processes, such as skeletal, cardiac, and smooth muscle contraction, blood clotting, and nerve impulse transmission, to name a few. Excitable cells such as neurons are sensitive to changes in calcium ion concentration, and an increase above normal (hypercalcemia) leads to a progressive decline in the nervous system. Conversely, a decrease in calcium concentration (hypocalcemia) leads to increased excitability of the nervous system. An important feature of extracellular calcium regulation (Calcium Metabolism) is that only about 0.1% of total body calcium is present in the extracellular fluid, about 1% is stored in cells and their organelles, and the remainder is stored in bone. Thus, bones act as large reservoirs that store excess calcium and release it when the concentration of the extracellular fluid decreases.
The body's distribution of calcium is as follows:
Calcium Metabolism- The mineral makes up 99% of teeth and bones, or 2% of body weight. The remaining 1% is distributed among various tissues as follows: Muscle: 8 mg per 100 g of fresh muscle tissue. Serum or plasma: 9–11 mg/100 ml RBC minute track. Lymph and aqueous humor (as well as ascites and edema fluid) contain slightly less than plasma. Cerebrospinal fluid: 5.3 mg per 100 ml. Maternal sources during fetal life: Very little calcium is detectable in the fetus until the fifth month of intrauterine life, as bone formation begins. During the last two months of intrauterine life, when rapid and extensive ossification occurs, more than 60% of the total calcium deposits are deposited.
Calcium in plasma and interstitial fluid :-
Calcium Metabolism- Calcium in plasma exists in three forms, About 41% of the calcium (1 mmol/L) is bound to plasma proteins and may be present in this form, which does not diffuse through the capillary membrane; About of calcium (0.2 mmol/L) can diffuse through the capillary membrane, but is not ionized because it is associated with anionic substances (such as citrate and phosphate) in the plasma and interstitial fluid; The remaining 50% of calcium in plasma diffuses through the capillary membrane and is ionized. Thus, the normal calcium ion concentration in plasma and interstitial fluid is about 1.2 mmol/L (2.4 mEq/L because it is a divalent ion), which corresponds to half of the total plasma calcium concentration. This ionic calcium is the form that is important for most of the functions of calcium in the body, including calcium’s effects on the heart, nervous system, and bone formation.
Sources :-

Water (especially hard water), eggs, milk (about 1g per litre), cheese (5-10 g per kg) and green vegetables
are the main sources. Fish and meat are poor sources.
Daily Calcium Requirements-
• 1-3 years = 500 mg
• 4-8 years = 800 mg
• 9-18 years = 1,300 mg
• 19-50 years = 1,000 mg
• 51 years and older = 1,200 mg
• Pregnant women and mothers = 1,300mg
Site of Absorption :-
Calcium Metabolism- Absorption occurs primarily from food (especially dairy products) in the upper part of the small intestine (maximum in the duodenum) where vitamin D (present in food or by exposure to ultraviolet light) is absorbed; excess intestinal lipids reduce calcium absorption. Form of Absorption: Soluble inorganic forms are absorbed much better. Organic calcium in foods may be converted to inorganic forms before being absorbed. Insoluble calcium compounds are never absorbed. As a result, when phytic acid is present in cereals, insoluble calcium phytate is formed. Oxalates may have a similar effect. Calcium phosphate is not absorbed.
Regulation of blood calcium levels :-
Blood calcium levels (Calcium Metabolism) are regulated primarily by three hormones:
1. Parathyroid hormone
2. 1,25-dihydroxycholecalciferol (calcitriol)
3. Calcitonin
1. Parathyroid hormone is a protein hormone secreted by the parathyroid gland. Its main function is to increase blood calcium levels (Calcium Metabolism) by mobilizing (absorbs) calcium from bone.
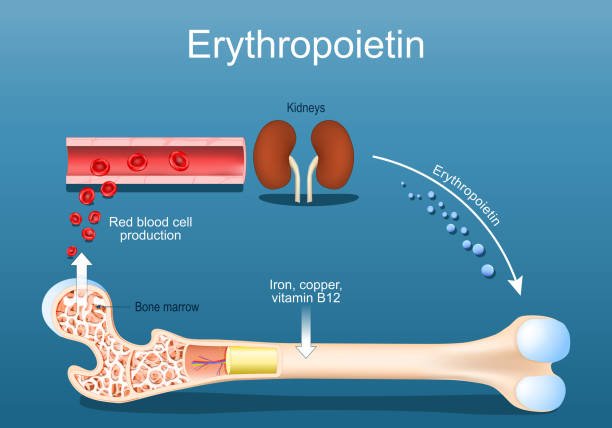
2. 1,25-Dihydroxycholecalciferol – Calcitriol Calcitriol is a steroid hormone synthesized in the kidneys. It is vitamin D in its activated form. Its main action is to increase blood calcium levels (Calcium Metabolism) by increasing calcium absorption from the small intestine.
3. Calcitonin- This hormone is secreted by the parafollicular cells of the thyroid gland. It is a hypo calcemic hormone. It lowers blood calcium levels (Calcium Metabolism) primarily by reducing bone resorption.
Factors Affecting Calcium Absorption (Calcium Metabolism) :-
1. Age: Infants and young children: Often absorb calcium more efficiently, promoting the development of strong bones.
Adults: Because calcium absorption (Calcium Metabolism) efficiency decreases with age, it is important to maintain adequate calcium intake from the diet.
Elderly: Postmenopausal women and older men often experience a further decline in calcium absorption due to changes in hormone levels and gastrointestinal function.
2. Role of Vitamin D – Vitamin D is a group of fat-soluble secosteroids that enhance calcium absorption in the intestine. Vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) are the two most significant substances in this category. Diet and sunlight-induced cutaneous synthesis are the two most important sources of vitamin D for humans. Vitamin D is biologically inactive. The liver and kidneys convert vitamin D into its active metabolite form, which enhances the intestinal transit of calcium.
The liver enzyme 25-hydroxylase hydroxylates cholecalciferol to produce 25-hydroxycholecalciferol.
In the kidney: 25-hydroxycholecalciferol is hydroxylated in the presence of the enzyme 1-α-hydroxylase to form 1,25-dihydroxycholecalciferol.
3. Protein content of the diet: Increasing protein intake improves calcium absorption. The most effective are amino acids lysine and arginine,
4. Phosphorus content of food: High phosphorus content in food leads to the formation of insoluble calcium phosphate , which reduces calcium absorption.
5. Sources of Calcium: Calcium from different sources is absorbed in different ways. Calcium from milk is highly absorbed, whereas calcium from plant sources is very poorly absorbed. Certain vegetables like spinach have high oxalate content, which converts soluble dietary calcium into insoluble calcium oxalate. As a result, these oxalate-containing veggies decrease the absorption of calcium.
6. Intestinal reactions: High acidity promotes calcium absorption because calcium salts become soluble in acidic medium. Alkalinity produces insoluble calcium salts, reducing absorption. Sugars, especially lactose, increase acidity by conversion to lactic acid, promoting calcium absorption. Excessive unabsorbed fatty acids in the intestine convert soluble calcium to insoluble calcium soaps, reducing absorption. Phytic acid, found in large amounts in grains, causes calcium to be excreted in the intestine as insoluble calcium phytate, reducing absorption.
Excretion of Calcium :-
During passage through the kidney, large amounts of calcium are filtered at the glomerulus. The renal tubule reabsorbs 98% to 99% of the filtrate’s calcium back into the circulation. The urine only excretes trace amounts. The urine only excretes trace amounts. Most of the filtered calcium is reabsorbed in the distal convoluted tubule and the proximal part of the collecting duct. In the distal tubule, parathyroid hormone increases reabsorption. In the collecting duct, vitamin D increases reabsorption and calcitonin decreases it. Approximately 1,000 mg of calcium is excreted daily, of which 900 mg is excreted in the feces and 100 mg in the urine.
Functions of Calcium :-
The body depends heavily on calcium. Here is a brief summary:
1. It is necessary for the development of teeth and bones.
2. It is essential for blood clotting.
3. It is essential for the clotting of milk.
4. It is essential for myocardial contraction and heart rhythm.
5. It maintains normal neuromuscular excitability. In this respect, it is the opposite of sodium and potassium, which are neuroexcitatory, whereas calcium is neurocalcific. Thus, hypocalcemia does not impede the action of sodium and potassium. The nervous system becomes highly excitable, resulting in convulsions, tetanus, etc.
6. Controls the permeability of capillary endothelium. High blood calcium levels decrease permeability, and low blood calcium levels increase permeability.
7. Activation of enzymes. Certain enzymes such as succinate dehydrogenase, ATPase, and lipase are activated by calcium.
Effects of Calcium Deficiency :-
The consequences of a calcium deficit include rickets and tetany. Inappropriate mineralization of bones results from a diet deficient in calcium or from inadequate calcium absorption brought on by low vitamin D levels. This condition is called rickets and usually occurs in children with a poor diet, especially one that is deficient in calcium and phosphorus. Renal rickets is caused by a tubular defect in the kidney that prevents normal reabsorption of calcium from the tubular filtrate, causing large amounts of calcium to be excreted in the urine. Because the defect is in the tubules, this phenomenon cannot be corrected by administering vitamin D.
