Pulmonary Circulation
Introduction :-
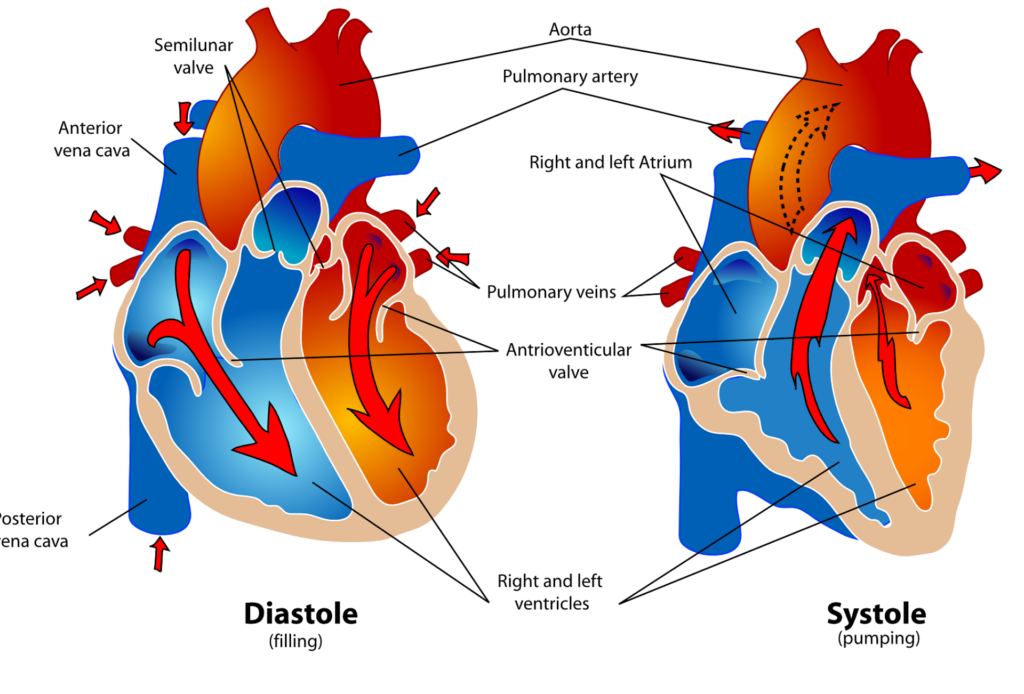
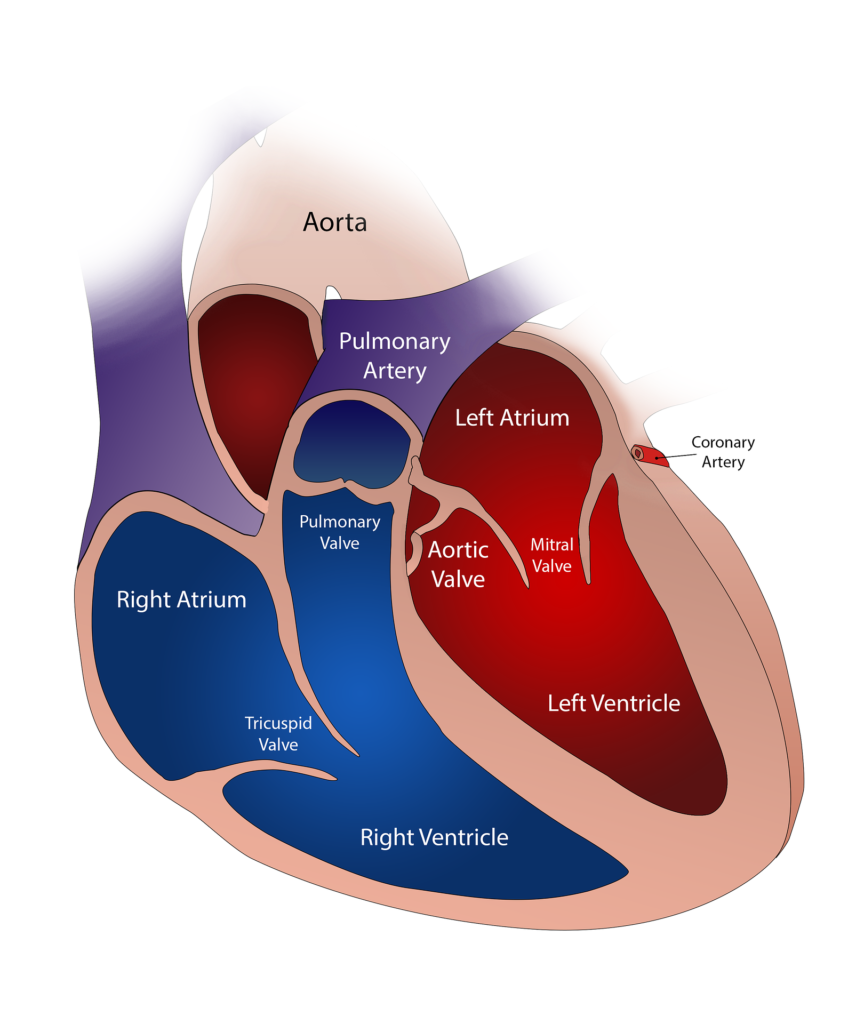
Pulmonary Circulation- The circulatory system’s pulmonary circulation is in charge of carrying blood with low oxygen content away from the heart and returning blood with high oxygen content from the lungs to the heart. There are two pathways by which blood can reach the lungs: the pulmonary and bronchial arteries. The pulmonary artery is more elastic and flexible than the aorta, although having the same cross-section. Blood from the venous system is transported by the pulmonary artery from the right heart to the lungs, where it absorbs oxygen and provides nutrition to the lung tissue.
Pulmonary Artery :-
Deoxygenated blood is delivered from the right ventricle to the lungs’ alveoli by the pulmonary artery (pulmonary circulation). This artery separates into left and right branches after entering the right ventricle. Each branch and principal bronchus enter the corresponding lung.
A branch of the pulmonary artery enters the lung, splits into smaller vessels, and eventually forms the capillary plexus, which is closely related to the alveoli. Alveolar gas exchange is the only function of the capillary plexus.
One pulmonary vein from each side carries oxygenated blood from the alveoli to the left atrium.
Bronchial Artery :-
The aorta gives rise to bronchial arteries, which transport oxygenated blood to bronchi and bronchioles.
The pulmonary artery divides into broad arterioles and capillaries, encircling the alveoli, the site of gaseous exchange, in a dense network. Additionally, the bronchial artery divides into capillaries that return primarily via bronchial veins and somewhat by azygos veins, joining the alveolar network in part. The bronchial artery branches also exists in the walls of the bronchioles, bronchial glandular systems, and respiratory bronchioles. As a result, they produce capillary plexuses that allow blood to flow into the pulmonary venules. The pulmonary tissues receive their oxygen supply from both oxygenated and deoxygenated blood.
The descending thoracic aorta is the source of the bronchial arteries.
They supply arterial blood to the pulmonary lymph nodes, visceral pleura, bronchi, connective tissue, and other components of the pulmonary interstitium. Two bronchial veins on either side of these structures drain the venous blood within them. The left bronchial vein drains into the superior hemiazygos vein or left superior intercostal vein, and the right bronchial vein drains into the azygos vein. In the meantime, blood from distal areas of the bronchial circulation is immediately received by tributaries of the pulmonary veins.
Control Factors of Pulmonary Circulation :-
A number of variables work together to precisely control pulmonary circulation, which is necessary for effective gas exchange and stable blood levels of oxygen and carbon dioxide. The following are the main pulmonary circulation regulating factors.
1. The right ventricle’s output (mechanical factor) is determined by the frequency, force, and degree of venous return during contraction. Although cardiac output may increase three or four times, there is no discernible increase in pulmonary arterial pressure.
2. The pulmonary bed’s resistance is contingent upon the subsequent factor: (a) Pulmonary vasoconstriction is caused by hypoxia in the lung lumen. The pulmonary blood vessels contract when blood CO2 tension rises. The majority of blood is observed to be transferred to the lung that is ordinarily ventilated in order to protect the body from the hypercapnoic effect, if one lung is ventilated with a mixture of CO2 and O2, and the other lung with air. This is the pulmonary blood flow auto-regulation.
(b). Acid-base balance: Changes in blood pH, such as acidosis (low pH) or alkalosis (high pH), can affect pulmonary vascular tone.
3. Autonomic neural system: The pulmonary vascular tone is regulated by the parasympathetic and sympathetic nervous systems.
Vasoconstriction brought on by sympathetic activation may raise resistance and pulmonary arterial pressure.
Vasodilation brought on by parasympathetic activation may lower pulmonary arterial resistance and pressure.
4. Additionally, noradrenaline and adrenaline cause vasoconstriction. The pulmonary blood vessels widen in response to acetylcholine as well, however the extent of this dilation is primarily determined by the pre-existing tone of the pulmonary blood vessel’s smooth muscle.
The humoral chemical serotonin, which is produced by chromaffin tissue secretory products or disintegrating platelets, also narrows the blood arteries in the lungs.
5. Function of respiration: More blood enters the lungs during inspiration due to the pulmonary bed’s enlargement and a drop in capillary pressure to around 2 mm Hg. The capillaries elongate as a result of stretching, and they dilate as a result of negative pressure and maybe a vasomotor impact. As a result, the lungs may store 10% of the entire blood volume during inspiration. During expiration, the lungs can only hold around 6% of the blood volume due to reversal changes that occur and a pressure increase of approximately 4 mm Hg.
But during forced deflation as well as peak lung inflation, total pulmonary vascular resistance rises. The essential capacity measurement serves as a plan of action. Pulmonary congestion during a fall.
6. Reflex control: Reflexes present in the sinoaortic region caused by stimulation of baroreceptors also affect the pulmonary circulation. In the pulmonary vascular bed, stimulation of baroreceptors in the carotid sinus and aortic arch results in reflex vasodilation, whereas stimulation of chemoreceptors in the carotid artery or aortic body results in pulmonary vasoconstriction.
Normal Pulmonary Circulation Values :-
Ensuring optimal gas exchange and general cardiovascular health requires normal pulmonary circulation parameters.
1. Pulmonary Artery Pressure (PAP): The normal human pulmonary artery has a systolic pressure of roughly 22 mm Hg (approximately 22 mm Hg in the right ventricle). About 10 mm of mercury is the diastolic pressure (right ventricle O to 1 mm of mercury). These vessels pulse as a result of the pulmonary artery’s increasing pressure with each heartbeat. About 8 mm of mercury is the pulmonary capillary pressure. roughly 5 mm of Hg is the pulmonary venous pressure (left atrium: roughly 4 mm of Hg).
2. Pulmonary Capillary Wedge Pressure (PCWP): Normal range: 6 to 12 mmHg
This value reflects the pressure in the left atrium and is useful for assessing left ventricular function.
3. Mixed Venous Oxygen Saturation (SvO2): Normal Range: 60-80%.
This number represents the equilibrium between the supply and consumption of oxygen and shows the saturation level of oxygen of blood returning to the lungs.
4. Blood oxygen pressure in the vessels (PaO2): Range of Normal: 75-100 mmHg.
The partial pressure of oxygen in arterial blood is indicated by this value.
5. Arterial Carbon Dioxide Pressure (PaCO2): Normal Range: 35-45 mmHg
This value measures the partial pressure of carbon dioxide in arterial blood.
6. Arterial Blood Oxygen Content (CaO2): Normal Range: 16-20 ml of oxygen per 100 ml of blood (ml/dl)
This value reflects the total amount of oxygen in the blood, including dissolved oxygen and oxygen bound to hemoglobin.
Pulmonary Circulation Functions :-
The pulmonary circulation is a key component of the cardiovascular system and serves several important functions in maintaining overall health and homeostasis.
1. Gas exchange: The pulmonary circulation’s primary purpose. Gastronic exchange occurs across the alveolar airway and alveolar capillaries when mixed, blood that is deoxygenated is circulated via alveolar capillaries. Gaseous exchange allows blood traveling via alveolar capillaries to exchange the appropriate amount of CO2 with oxygen.
2. Filter: A filter is provided by the tiny pulmonary blood channels.
The emboli that enter the pulmonary capillaries are caught by it. As a result, the filter keeps the heart and brain’s blood arteries from being reached and clogged.
3. Nutrition: Lung tissue is kept nourished by the pulmonary circulation.
4. Fluid exchange: Because the pulmonary arterial pressure is so low, fluid tends to be drawn out of the alveoli, and any fluid that builds up there is quickly taken up by the blood.
5. Left ventricle reservoir: Blood return from the pulmonary bed to the left atrium is the only factor influencing left ventricular output. Therefore, any change in the pulmonary hemodynamics will also affect the function of the left ventricle.
